
At Mast Cell Action, we are committed to supporting those living with Mast Cell Activation Syndrome (MCAS) and raising awareness about this complex condition. But we can’t do it alone.
We’re inviting our community to get involved in a way that feels right for you. There are many ways you can make an impact:
Do you have contacts within healthcare, media, or other networks that could help us spread the word or collaborate on initiatives? We'd love to hear from you.
Every contribution helps us provide crucial resources and support for individuals affected by MCAS. You can support us by donating, fundraising, or even dedicating an event or challenge to raise awareness and funds.
Your generosity and connections can make a world of difference to those facing MCAS. Thank you for being part of our community and helping us continue this vital work.

What is Mast Cell Activation Syndrome?
Mast Cell Activation Syndrome (MCAS) is a condition which can develop in children or adults. MCAS forms part of a spectrum of mast cell disorders. People with MCAS may also have other mast cell disorders such as mastocytosis or hereditary alpha tryptasemia syndrome (HATS).
In people affected by MCAS, chemicals called mast cell mediators are released too frequently or abundantly, and/or in response to triggers that are not typically considered to be harmful, for example; foods or chemicals in the environment. This can lead to a wide range of symptoms that affect multiple parts of the body.
Triggers and symptoms of MCAS vary greatly between individuals. Triggers can include fragrances, exercise, stress and changes in temperature. MCAS symptoms can come and go and may often change over time within the same person. This can make it difficult to identify specific triggers, and the number of triggers and severity of symptoms may continue to increase as the condition progresses.
More research is needed to understand MCAS. Sometimes the condition occurs in family groups, suggesting that there may be genetic causes of MCAS. For example, HATS is a genetic condition caused by the presence of extra copies of the alpha tryptase gene (TPSAB1). Since the genetic causes of mastocytosis and HATS are well-characterised, genetic tests for these conditions are available.
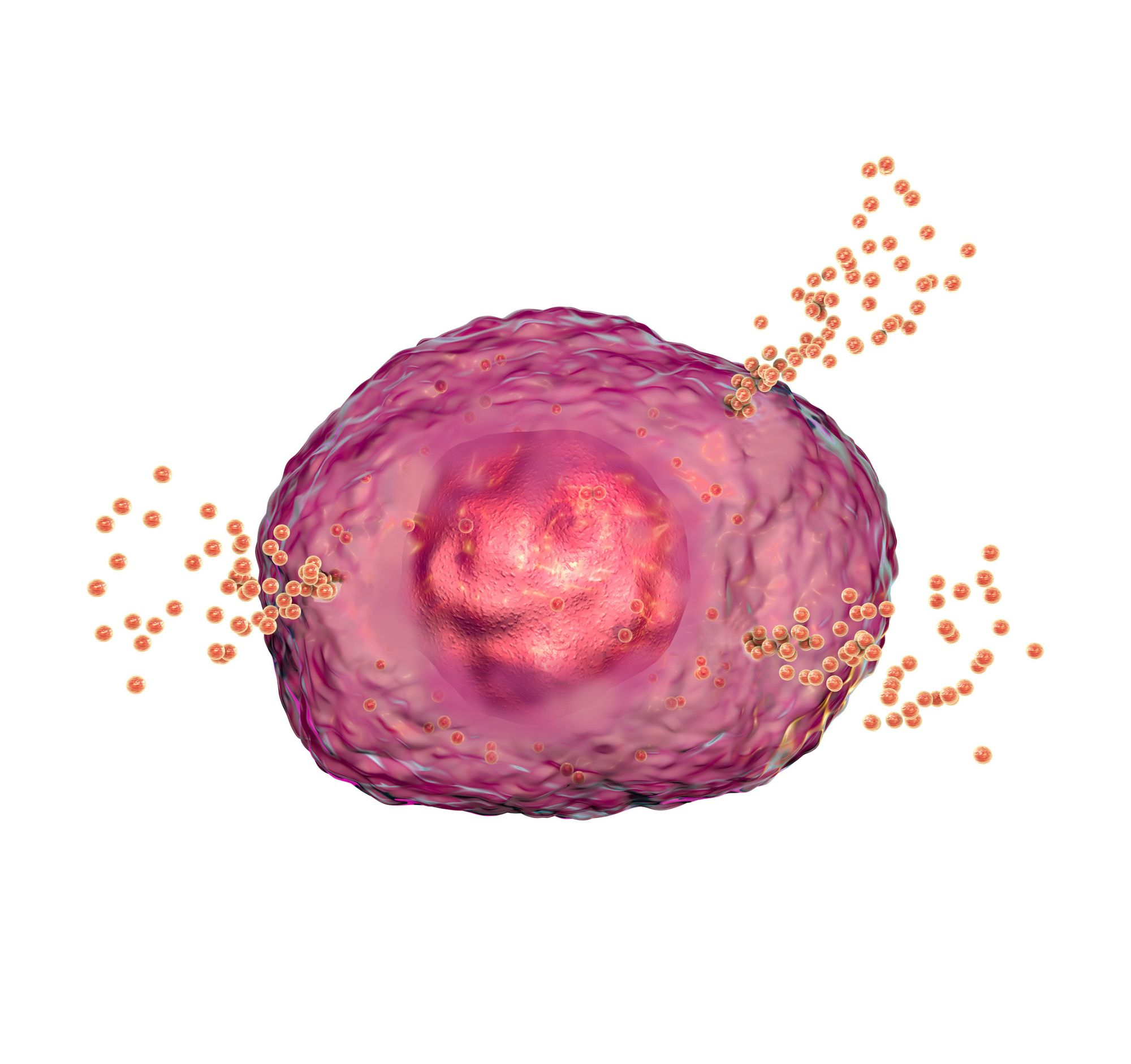
What is a mast cell?
Mast Cells are a type of blood cell found in all parts of the body. They are a key part of the immune system. Mast cells detect different types of triggers and tell other immune cells how to respond.
Mast cells are known as 'police officers’ of the immune system' – spotting signs of trouble and calling for back-up when needed.
In a healthy state, mast cell mediators create a number of protective responses in the body to help fight infection and promote healing. In someone with MCAS, where these mediators are released too frequently, they can affect the body in multiple ways - causing multiple symptoms in different parts of the body at the same time.
Usual mast cell triggers include bacteria, parasites, viruses, stings and wounds. Additional triggers for many people with MCAS include food and environment.

Mediators
Mediators include a mixture of chemicals that aid in boosting an immune response. Below are the most common mediators found in mast cells, but there are many, many more.
Histamine is one of the most well-known chemicals found within mast cells and is responsible for causing symptoms such as itching, swelling and redness which are often seen during allergic reactions. Cytokines are also found in mast cells, linked to wound healing and responding to infection, Cytokines act as a messenger, signalling and recruiting other immune cells to boost the effects of the immune system.
Tryptase is an enzyme which is mostly found in mast cells but is also found in many different parts of the body.
This is a type of protein that helps with chemical reactions and is also often seen in allergic reactions. When functioning correctly, these mast cell mediators keep your body healthy and strong, however, in those with MCAS, these mediators and mast cells, are very sensitive and overly active. This results in many different symptoms, some of which can be very serious.
Many different things can trigger these reactions, so identifying and avoiding (where possible) each person's individual triggers is an essential part of managing MCAS.

How is MCAS diagnosed?
We know how important getting a confirmed diagnosis of MCAS can be. Published guidance recommends four diagnostic stages that should be completed so that your doctor feels comfortable confirming a full diagnosis of MCAS. Getting this diagnosis can be a complex and lengthy process taking many years, particularly due to the challenges involved with testing for mast cell mediators.
Stage 1
MCAS is considered a multi-systemic condition, which means that two or more body systems are affected at the same time during a reaction. Because of the complex pattern of symptoms, no two people are likely to experience MCAS in exactly the same way. Symptoms can also vary over time, often waxing and waning.
It is common for someone with MCAS to have mild and controllable symptoms for a long time, but a stressful event like an infection, an operation or an illness – for example COVID-19 – can cause a dramatic increase in symptom severity or frequency. Again this can make recognising the symptoms of MCAS quite challenging.
Stage 2
This stage ascertains if MCAS symptoms are improving with certain medications. This may be referred to as a medication trial - if a person’s symptoms get better after taking a known MCAS medication, then a diagnosis is more likely.
You can find out more about MCAS medications here.
Stage 3
There are tests that can be used to identify whether higher than normal levels of chemical mediators are present in the body. These mediators can be tested for in the blood or in the urine.
Due to the allergic-type symptoms of MCAS, testing for IgE-mediated allergies is often one of the first tests to be performed by doctors, usually as a skin prick test or by taking a blood sample for RAST testing. In idiopathic MCAS these are usually found to be inconclusive or negative.
A blood test to evaluate tryptase levels is often performed, particularly as it is a strong marker for mastocytosis and for HATs, but it is considered less specific for MCAS as many people affected by MCAS do not have high baseline tryptase levels. This means that their normal, everyday tryptase levels are not high. They may however be higher during a symptom flare or during anaphylaxis, but it can be challenging to obtain blood samples at this precise time for testing.
Other mast-cell mediators can be tested for with a 24-hour urine collection. These include methylhistamine and prostaglandins. Elevated results of these can be suggestive of MCAS but having normal levels doesn’t rule out MCAS and repeated testing may be needed.
It is often better to take these tests during a flare, when symptoms may be particularly severe. In addition, some tests may need to be performed in the absence of particular medications, which will need to be carefully discussed with a health professional. However, we know that for some people it can be difficult to choose to stop treatment, particularly when it is effective, and this is an important consideration when seeking a fully ‘biochemically-confirmed’ diagnosis.
Biopsies can also be taken from the gut, bladder or skin, where the presence of high or abnormal mast cell numbers can be supportive of a diagnosis of MCAS or mastocytosis.
Unfortunately, there are currently no genetic tests identified for diagnosing MCAS – but research is underway to change this.
Stage 4
Eliminating any other possible causes of symptoms is an important stage of the diagnostic process as there are many conditions that overlap with MCAS such as ME/CFS, Lyme, and asthma, for example.
Due to the wide-ranging symptoms associated with MCAS there can be an overlap with the symptoms experienced with a number of other conditions. During any diagnostic process, it is important to ensure that other potential diagnoses are not missed. In addition, more than one condition can exist at the same time. This may mean additional investigations such as endoscopy, colonoscopy, imaging and biopsies are required.
As MCAS may not have been the first thing that your doctor suspected, you may have undergone some of these tests already. We appreciate that this can be frustrating, and some tests can be unpleasant, but it can help to remember that for a confirmed diagnosis of MCAS it is important that other potential diagnoses have been excluded.
Other conditions that are important to rule out include heart attacks, hepatitis, cancer, epilepsy, oesinophilic oesophagitis, Addison’s disease and diabetes.

Anaphylaxis
People who have MCAS are at an increased risk of having an Anaphylactic reaction after encountering a trigger. Anaphylaxis is a potentially life-threatening allergic reaction, it has a rapid onset of symptoms and it is important to be aware of the ABC signs:
Airways: look for a persistent cough, swollen tongue or lips, and difficulty swallowing.
Breathing: look for difficulty breathing and wheezing.
Circulation/Consciousness: look for reduced blood pressure, confusion, and collapsing.
Pre-loaded adrenaline auto-injectors, commonly known as EpiPens, are prescribed to combat anaphylaxis. If you are at risk of anaphylaxis you need to carry your auto-injector at all times, and give an injection as soon as any symptoms of anaphylaxis occur. Always call an ambulance immediately following injection, even if there is a drastic improvement.

Comorbidities
People who have MCAS often have at least one additional condition.
Common comorbidities include connective tissue disorders such as Ehlers Danlos Syndrome (EDS) and Marfans, dysautonomia, such as postural orthostatic tachycardia syndrome (POTS), and type 2 diabetes.
The relationship between MCAS and many of these comorbidities is yet to be fully understood, and more research is required.
Further information on comorbidities can be found in the Royal College of GPs Ehlers Danlos Syndromes Toolkit.
You can read more about comorbidities here.

Casper the Chameleon
We are delighted to have published a children's book, Casper the Chameleon. Written by our very own Director of Operations, Joy Mason.
Order your copy for free by completing this form.
We hope that our other resources will be used in partnership with the book to support wellbeing in the MCAS community.
The book was created thanks to our Wellbeing Fund. The fund is designed to create sustainable resources to continue to benefit the wellbeing of our community, targeting new initiatives and improving existing offerings to unleash significant positive impact.
Can you help?
We have many plans to support those living with MCAS and with your support, we can do so much more! Every pound you donate will support people with MCAS, as well as their families, doctors and researchers. Your donation will help us to develop resources and support to help many individuals in our community.
£10 could send a Casper pack to help a child living with MCAS to feel less alone & share their feelings.
£25 could help to support people with MCAS and their families through our dedicated peer support groups.
£100 could support our work to develop and distribute a range of wellbeing and self-management resources for adults with MCAS.
You can donate here.
"I have only just found Mast Cell Action and it offers a lot of support that the NHS and my consultant haven’t offered. I have had so many questions answered and different ways of adapting suggested, that I have needed without realising."
Become a friend
Sign up to become a Friend of Mast Cell Action so we can keep you up to date on our progress and on how to get involved in our latest campaigns and initiatives.
Donate
Mast Cell Action relies entirely on the generosity of people like you. Please make a donation now and together we can make a difference to those affected by MCAS.







