
MCAS and Histamine Intolerance
Mast Cell Activation Syndrome (MCAS) and histamine intolerance are frequently mistaken for each other because they share many overlapping symptoms, such as headaches, flushing, digestive issues, and itching.When considering a low histamine diet, it’s essential to look at your specific symptoms and reaction patterns.
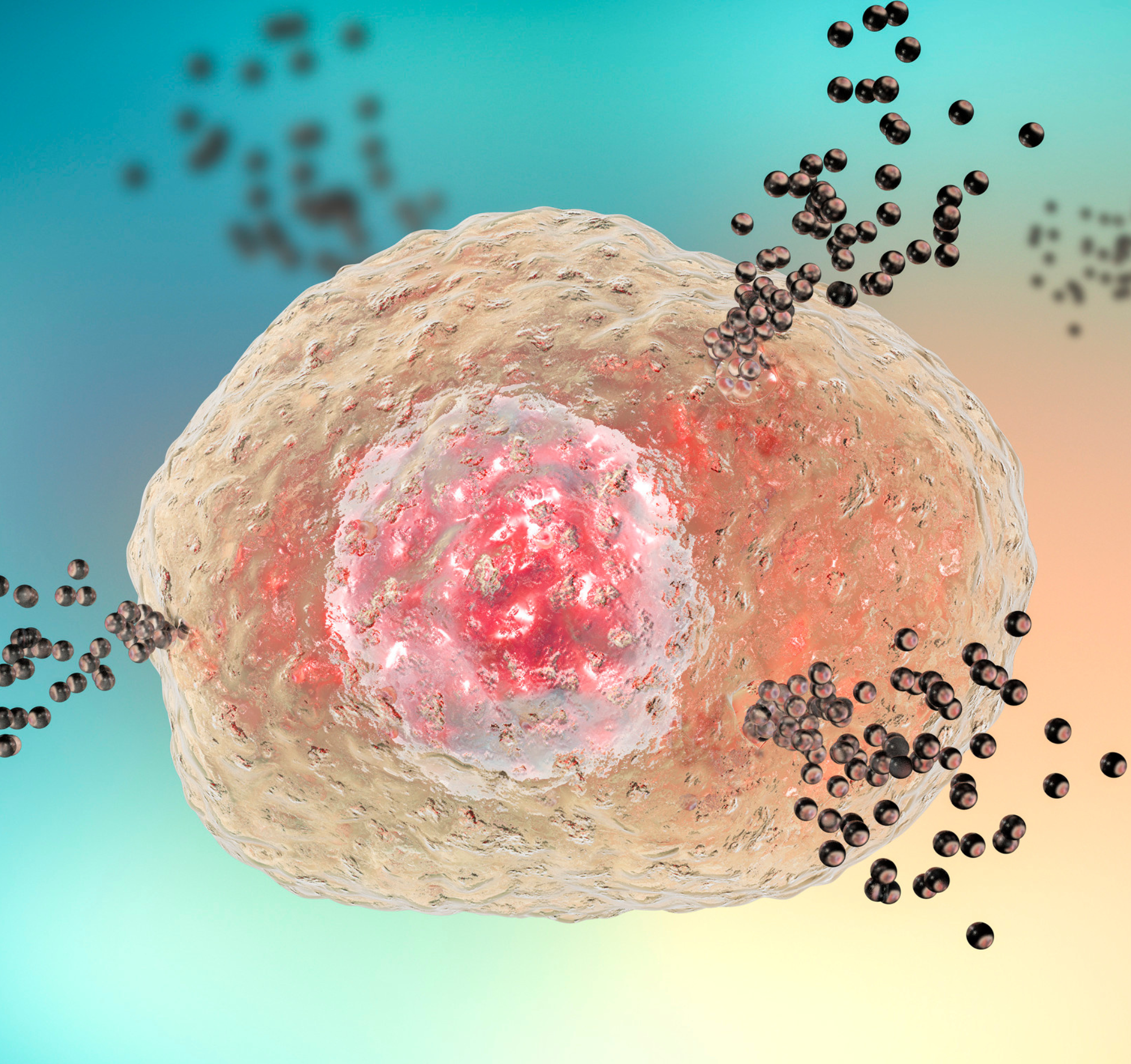
MCAS involves the abnormal release of various mediators (not just histamine) from mast cells, which can cause a wide range of symptoms across multiple body systems. While histamine is one of these mediators, MCAS also involves others like tryptase, prostaglandins, and leukotrienes, which can trigger different reactions. As a result, someone with MCAS may not necessarily react to dietary histamine, as their symptoms could be driven by other substances released from their mast cells.
Histamine intolerance, however, specifically refers to a reduced ability to break down histamine from dietary sources due to factors like low levels of the enzyme diamine oxidase (DAO). This causes a buildup of histamine in the body, leading to symptoms that are primarily related to excess histamine, such as nasal congestion, hives, and digestive discomfort.

Determining the Need for a Low Histamine Diet
When considering a low histamine diet, it’s crucial to assess which symptoms you’re experiencing and whether they align more with histamine intolerance, MCAS, or a combination of both. This understanding can help guide dietary adjustments and ensure you’re targeting the right triggers.
Assess your symptoms to determine if a low histamine diet is necessary. Not everyone with MCAS will benefit from such a diet. Identifying patterns in your reactions can help decide if histamine is a factor. You could use our symptom log to keep track.
Avoid restricting foods unless absolutely necessary. It’s beneficial to track symptoms and foods to pinpoint specific triggers rather than broadly eliminating foods from your diet.

Implementing a Low Histamine Diet
It’s generally recommended to try a low histamine diet for a short period, typically two weeks. If there’s no noticeable improvement within this time, it might not be worth continuing, unless there are known delayed reactions, in which case, extending to four weeks could be considered.
Rather than a strict low histamine diet, consider histamine modification. This approach allows for more flexibility and control, letting you adjust histamine levels in your diet according to your tolerance and needs.
Adapt the diet to your personal needs. Some people might benefit from reducing histamine by making small adjustments, such as avoiding leftovers or freezing foods immediately, rather than adhering to a strict low histamine diet, especially if they have other dietary restrictions or are underweight.

Reintroducing High Histamine Foods
When reintroducing high histamine foods, do it gradually. Start with a small portion on day one, double it on day two, and triple it on day three. This method helps to monitor reactions in a controlled manner. Consider your nutritional needs and personal preferences when reintroducing foods. Focus on foods that are nutritionally important or those you miss the most.
Overcoming fear of reintroducing foods can be challenging. Building confidence through successful reintroductions helps. Start by touching the food to your skin, then to your lips, before finally eating it.
Reducing stress during reintroduction is crucial. Techniques like mindfulness, meditation, or even listening to music can help create a calming environment. Distraction from hyper-focusing on symptoms can also be beneficial.

Summary
Managing histamine intolerance and its associated symptoms, such as brain fog and attention problems, involves a multifaceted approach.
You could consider DAO enzyme supplements if not already in use and/or continue a low-histamine diet if it helps, while ensuring nutritional adequacy.
Experiment cautiously with food reintroduction under stable health conditions and diversify your plant-based food intake to support gut health without relying solely on fermented foods.
Where possible, seek comprehensive testing and medical advice to rule out other potential conditions and to receive tailored treatment recommendations.

Conclusion
Living with MCAS presents unique challenges, especially regarding diet and food tolerance.
Continuously reintroducing foods cautiously and seeking the right professional support are key strategies for managing your condition effectively.
Always prioritise safety and professional guidance in your journey towards expanding your diet and improving your overall health.
We hope you find the following Q&A useful.
Food Reintroduction and Restricted Diets
Should I Continue Trying to Reintroduce Foods?
Reintroducing foods can be beneficial, but it depends on several factors, especially the type and severity of your reactions. Reactions can vary greatly, from skin symptoms and gut issues to anaphylaxis. Below are some things that you should consider before and during reintroduction of foods.
- Identify whether your reactions are mild, moderate, or severe (e.g., anaphylaxis). If severe, avoid home reintroduction and seek medical supervision.
- Consider the timing of reintroductions. Factors like stress levels, pollen season, and current medications can influence your reactions. Choose a stable period in your life to try new foods.
- Start with foods similar to those you can already tolerate. This gradual expansion can be safer and more manageable. Look for patterns in the types of foods you react to. Building on foods with similar chemical compositions can help.
- Test a new food multiple times before concluding whether it’s safe or not. External factors can sometimes cause temporary reactions.
- Maintain a detailed food diary to track food intake and reactions. This helps identify patterns and potential triggers.
- Always consult with healthcare professionals when planning food reintroduction to ensure it's done safely.
Should I Reintroduce Dairy After 20 Years of Avoidance Due to Severe Diarrhea?
Reintroducing dairy after a long period of avoidance requires careful consideration:
- It’s important to determine the original cause of the severe diarrhea. Comprehensive medical evaluation, including stool tests for gut inflammation and other diagnostic tests, is essential.
- Dairy isn’t the only source of calcium. Plant-based alternatives, fortified foods, and certain vegetables can provide adequate calcium. Refer to resources like the British Dietetic Association’s guide on calcium sources to ensure you’re meeting your nutritional needs.
- If you decide to reintroduce dairy, start with very small amounts to monitor your body's reaction. This gradual approach helps identify if dairy is the culprit and prevents severe reactions.
- Always discuss with your doctor or dietitian before making dietary changes, especially after such a prolonged period of avoidance.
Finding and Working with a Specialist Dietitian
How Can I Access a Dietitian Specialised in MCAS?
Accessing a dietitian with expertise in MCAS can be challenging due to the lack of specialised services.
If your referral has been rejected, find out why. It might be due to the absence of commissioned MCAS services, leading to a lack of skilled dietitians in this area.
Consider a referral based on your predominant symptoms. For example, if you have gastrointestinal issues, seek a gastroenterology dietitian. They may not be MCAS specialists but can manage related symptoms effectively.
Many dietitians are willing to educate themselves on MCAS if they are unfamiliar with it. Providing them with resources and information can help them assist you better. You can refer them to our resources for Healthcare Professionals. Encourage your current healthcare providers to collaborate with dietitians and share information on MCAS. This team approach can improve your care.
What Advice Do You Have on a Low Histamine Diet for a Child?
Implementing a low histamine diet for children requires careful consideration due to their complex nutritional needs and growth requirements. Here are key points to keep in mind:
Consult a Dietitian: It's crucial to work with a dietitian, especially one experienced with children. Their needs are more intricate, and professional guidance ensures they receive adequate nutrition for growth and development. There are additional factors such as fussy eating and social situations (e.g., school meals, parties) that can complicate dietary management.
Gradual Dietary Changes: Instead of immediately implementing a strict low histamine diet, consider starting with a "light" version. For example, if tomatoes are suspected to cause issues, remove only tomatoes initially and monitor the child’s response. This approach minimises unnecessary dietary restrictions and potential nutritional deficiencies.
Specialised Services: In the UK, there are specialised services available for children with complex dietary needs. For instance, the Leicestershire service offers a children’s dietitian, and local referrals to such centres can be beneficial.
Impact of Highly Restricted Diets on Health
Can a Very Restricted Diet Make Symptoms Worse?
Yes, a highly restricted diet can potentially worsen symptoms for several reasons:
Gut Microbiome Health: A diverse diet supports a healthy gut microbiome. Restricting too many foods can disrupt this balance, negatively impacting gut health and potentially exacerbating histamine intolerance and other symptoms.
Nutritional Deficiencies: Eliminating multiple foods can lead to deficiencies in essential vitamins and minerals, affecting overall health and the body's ability to manage histamine. For example, the enzyme that breaks down histamine requires specific nutrients to function efficiently. Without these nutrients, histamine levels may increase, worsening symptoms.
Psychological Impact: The stress of maintaining a highly restrictive diet can have psychological effects, including increased anxiety about food. This stress can trigger or worsen physical symptoms, creating a cycle of fear and avoidance that makes reintroducing foods even more challenging.
I've Been Living on a Highly Restricted Diet of Boiled Potatoes, Honey, and Water for Years. Any Suggestions?
First, it's essential to confirm and understand the specific nutrient deficiencies through testing. Addressing these deficiencies is crucial for improving overall health and gut function. Work with a healthcare provider to test for specific nutrient deficiencies. This will help tailor a supplementation plan to correct these deficiencies.
Start with foods closely related to the ones you can tolerate. For example, if you can tolerate certain seeds, try introducing other seeds or nuts one at a time. Reintroduce foods that are least likely to cause a reaction. This often includes foods similar in composition to those you already tolerate.
Seek a dietitian who can support the reintroduction process. Even if NHS resources are limited, if you can, consider private consultations or specialised services.
Keep a detailed food diary to track any reactions and adjust the reintroduction process accordingly.
Use supplements to address specific deficiencies as advised by your healthcare provider, especially during the early stages of food reintroduction.
Histamine Intolerance and Sleep Management
I Wake Up Frequently at Night and Found Some Benefit with a Low Histamine Diet. Any Suggestions to Improve Sleep?
Histamine can directly affect sleep, and managing mast cell activation syndrome (MCAS) holistically can help. Here are some strategies:
Sleep Hygiene:
- Establish a calming bedtime routine.
- Minimise exposure to screens and bright lights before bed.
- Ensure your sleep environment is comfortable and conducive to rest.
Stress Management:
Incorporate stress-relief techniques such as meditation, deep breathing exercises, and yoga into your daily routine. You can find some relaxing shorts on our YouTube channel.
Gut Health:
- Incorporate as many tolerated plant-based foods as possible to support gut microbiome health.
- Introduce high-fiber foods like whole grains, fruits, vegetables, nuts, and seeds to stabilise gut bacteria.
- Consider the timing of caffeine intake, as it can affect both histamine levels and sleep quality. Some may benefit from decaffeinated options.
- If prescribed, taking antihistamines at night can help due to their sedative effects, improving sleep.
How Can I Manage My Severe Brain Fog and Attention Problems Caused by Histamine Intolerance, and How Can I Reintroduce Foods Without Worsening My Symptoms?
If you're not taking DAO supplements, they might help manage histamine levels from food. DAO enzymes can break down histamine before it affects your system. Some studies suggest that DAO supplements, especially those derived from pig kidney extract, can be beneficial if taken before meals.
DAO Levels and Symptoms:
Blood DAO levels might not accurately reflect gut DAO levels. Therefore, basing decisions solely on blood DAO levels isn't advisable.
If your symptoms improve on a low-histamine diet and your nutrition is adequate, you might consider continuing the diet while monitoring and reviewing your health status periodically.
The link between consuming certain foods (like tomatoes) and symptoms such as uveitis might be coincidental. It's essential to test reintroduction cautiously and ideally under optimal health conditions.
There's confusion regarding fermented foods due to their high histamine content. Not everyone with histamine intolerance reacts to the same degree. Finding your personal threshold is crucial. Supporting your gut microbiome doesn't solely rely on fermented foods. Incorporating a variety of plant-based foods (whole grains, fruits, vegetables, nuts, seeds, beans, pulses, spices, and herbs) can also be beneficial.
Aim for a diverse intake of plant-based foods (e.g., 30 different types of plants per week) to support gut health positively and manage histamine levels effectively.
If you experience symptoms like uveitis, it might indicate an autoimmune condition rather than being solely related to histamine intolerance. Consultation with a healthcare professional is essential for proper diagnosis and treatment.
Hormonal changes can significantly impact symptoms related to gut health and histamine intolerance. Times of hormonal fluctuations, such as childbirth, can exacerbate symptoms.
It is important to have thorough testing (e.g., for celiac disease and other gut conditions) to understand the underlying causes of your symptoms and to ensure optimal management strategies.
Non-Medicated vs. Medicated Approaches to Histamine Intolerance
Is It Better to Treat Naturally Rather than Take Antihistamines?
It's not necessarily better to choose one approach over the other; rather, it’s about finding a balance that works for you. Many people use a combination of conventional medicine and natural approaches to manage histamine intolerance. Utilising both mainstream medical treatments and natural remedies often yields the best results. This allows you to address symptoms from multiple angles.
Antihistamines are generally safe and have been used effectively for many years. However, some individuals may react to antihistamines or the fillers in them. Your unique situation will dictate the best approach. Some might need medications due to severe symptoms, while others might benefit from natural methods.
Treatment plans vary significantly between individuals. It’s important to piece together a plan tailored to your specific needs and responses. A combination of treatments provides more options to manage symptoms effectively.
Can Mast Cell Activation Syndrome (MCAS) Cause Non-Diabetic Hypoglycemia and Reactive Hypoglycemia?
While there is no definitive evidence linking MCAS directly to reactive hypoglycemia, there is some overlap with conditions like Postural Orthostatic Tachycardia Syndrome (POTS), which can coexist with MCAS. Reactive hypoglycemia involves episodes of low blood glucose following meals, leading to symptoms like dizziness and shakiness. Here's how to manage and understand it better:
Symptoms of reactive hypoglycemia typically occur 2-4 hours after eating. These can be mistaken for autonomic symptoms due to similar sensations like shakiness and clumsiness.
Slow-Releasing Carbohydrates: Incorporate low glycemic index carbohydrates such as oats, boiled potatoes, and sweet potatoes. These foods release glucose slowly, preventing sharp drops in blood sugar levels.
Protein and Fat: Adding protein or fat to meals can help stabilise blood glucose levels.
Continuous Glucose Monitoring (CGM): While not always necessary, CGM can help understand blood glucose patterns, particularly for severe cases. However, professional interpretation of the data is crucial.
Medical Consultation: If you suspect reactive hypoglycemia, consult a doctor to rule out other causes and receive a proper diagnosis. Conditions like insulin resistance or other medical issues might need to be addressed.
Constipation and Gut Health in MCAS
What Is the Reason for Constipation in MCAS? Is It Because of Stomach Acid, Low Histamine Diet, or Undigested Food? And Can Magnesium Citrate Help?
There are many factors to consider when addressing constipation, particularly in the context of conditions like MCAS (Mast Cell Activation Syndrome):
Constipation can result from various factors such as:
- A limited diet can lack essential fiber and nutrients, contributing to constipation.
- Conditions like dysautonomia or Ehlers-Danlos Syndrome (EDS) can affect gut motility, causing slower transit.
- Irritable Bowel Syndrome (IBS) with constipation can be another unrelated cause.
There is no strong evidence linking low stomach acid directly to constipation. Discussions about low stomach acid and supplements are common online but lack scientific backing.
Seeing undigested food in stools, especially fiber-containing foods, is generally normal. It’s common to find some foods, like corn, partially undigested in stools.
People with hypermobility often experience delayed gut motility, leading to slower transit and constipation. MCAS can cause fluctuating bowel movements, ranging from constipation to diarrhea.
Magnesium Citrate and Alternatives:
While it can help with constipation, Magnesium Citrate might be too harsh for some individuals. It’s crucial to consider gentler options. There is evidence that magnesium oxide can increase the number of bowel movements per week. However, correct dosing is essential to avoid diarrhea. Professional advice on dosage is recommended to prevent adverse effects.
Definitions of constipation vary. It’s important to describe symptoms accurately to healthcare professionals. For example, having infrequent bowel movements, straining, or passing small, hard stools can all indicate constipation but require different management strategies.
While curcumin (found in turmeric) has anti-inflammatory and antioxidant properties, it is poorly absorbed in the gut. This limits its effectiveness in managing inflammation in chronic illnesses. Some supplements improve absorption with added lipids or fats, but it’s crucial to check for potential allergens like soy.
Any Tips for Cold Brew Drinks Without Artificial Flavorings and Sweeteners?
Here are some suggestions for cold brew drinks that are easy to prepare and free from artificial additives:
Herbal and Fruit Teas: Brew a variety of herbal teas such as chamomile, rooibos, or peppermint. These can be enjoyed hot or cold.
Fruit Infusions: Add slices of fruits like apple, cucumber, or berries to water for a naturally flavoured drink.
Cinnamon and Ginger: Where tolerated, add slices of fresh ginger or a stick of cinnamon to water for a subtle flavour boost.
Mint and Basil: Where tolerated, fresh herbs like mint or basil can add refreshing flavours to your water.
Flask of Tea: Prepare a flask of your favourite tea in the morning. This saves energy and ensures you have a ready supply throughout the day.
Chilled Herbal Teas: Brew herbal teas and store them in the fridge. They make for a refreshing and flavourful cold beverage.
Depending on individual sensitivity, you might prefer decaffeinated teas to avoid any potential histamine-related issues.
Become a friend
Sign up to become a Friend of Mast Cell Action so we can keep you up to date on our progress and on how to get involved in our latest campaigns and initiatives.
Donate
Mast Cell Action relies entirely on the generosity of people like you. Please make a donation now and together we can make a difference to those affected by MCAS.







